Essential Vitamins for Bones: Boosting Your Bone Health Naturally
Introduction to Healthy Bones
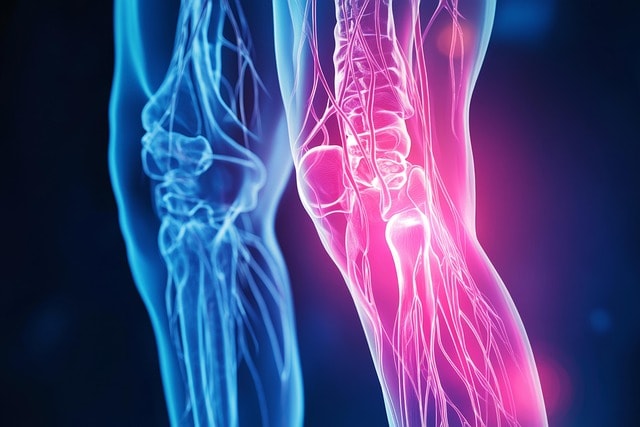
Bone health represents one of the most critical aspects of overall wellness, yet it’s often overlooked until problems arise. Our skeletal system serves as the structural foundation for our entire body, providing support, protection for vital organs, and serving as a reservoir for essential minerals. Understanding how to maintain and optimize bone health through proper nutrition, particularly through essential vitamins and minerals, can prevent debilitating conditions and ensure lifelong mobility and strength.
The human skeleton is a dynamic, living tissue that constantly undergoes a process called bone remodeling, where old bone tissue is broken down and replaced with new bone tissue. This continuous cycle requires a steady supply of nutrients to function optimally. Important nutrients such as calcium and vitamin D are vital for supporting strong bones and preventing bone loss. When nutritional needs aren’t met, the balance tips toward bone breakdown rather than bone formation, leading to decreased bone density and increased fracture risk.
Peak bone mass is typically achieved by age 30, after which bone density gradually declines. This makes early investment in bone health crucial, but it’s never too late to take action. Certain risk factors, such as age, hormonal changes, and deficiencies in calcium or vitamin D, can put individuals at higher risk for bone loss and fractures. The good news is that bones respond positively to proper nutrition and lifestyle interventions at any age, making bone health optimization an achievable goal for everyone.
Modern lifestyles often present challenges to optimal bone health, including sedentary behavior, limited sun exposure, processed food consumption, and inadequate intake of bone-supporting nutrients. A balanced diet is essential for providing the important nutrients needed to keep bones strong. These factors can accelerate bone loss and increase the risk of osteoporosis, a condition characterized by weak, brittle bones that fracture easily.

The Foundation: Calcium and Vitamin D Partnership
Calcium: The Building Block of Bones
Calcium stands as the most abundant mineral in the human body, with approximately 99% stored in bones and teeth. This essential mineral provides the structural framework that gives bones their strength and rigidity. Without adequate calcium intake, the body will extract calcium from bones to maintain critical functions like muscle contraction and nerve transmission, leading to progressive bone weakening.
The relationship between calcium intake and bone health is complex and influenced by numerous factors including age, gender, hormonal status, and the presence of other nutrients that affect calcium absorption and utilization. While calcium is undoubtedly crucial, it’s important to understand that simply consuming large amounts of calcium doesn’t automatically translate to stronger bones without proper supporting nutrients.
Daily calcium requirements vary throughout life, with increased needs during periods of rapid growth (childhood and adolescence), pregnancy and breastfeeding, and after menopause when hormonal changes accelerate bone loss. The recommended daily intake for adults ranges from 1,000 to 1,200 milligrams, depending on age and gender. It is important to get all the calcium your body needs from dietary sources, and if you are unable to meet these needs through food alone, a calcium supplement may be necessary to help maintain healthy bones, teeth, and muscle function.
Calcium absorption is a regulated process that becomes less efficient as intake increases. The body can typically absorb about 30% of calcium from food sources, but this percentage decreases when large amounts are consumed at once. This is why spreading calcium intake throughout the day is more effective than taking large doses in a single sitting. Consuming high-salt foods can cause the body to lose calcium, which may weaken bones over time.
Vitamin D: The Calcium Absorption Catalyst
Vitamin D functions more like a hormone than a traditional vitamin, orchestrating calcium absorption in the intestines and regulating calcium and phosphorus balance throughout the body. Vitamin D helps the body absorb calcium efficiently; without adequate vitamin D, the body can only absorb about 10-15% of dietary calcium, compared to 30-40% when vitamin D levels are optimal.
The relationship between vitamin D and bone health extends beyond calcium absorption. Vitamin D directly influences bone-forming cells (osteoblasts) and bone-resorbing cells (osteoclasts), helping maintain the delicate balance of bone remodeling. It also plays a crucial role in muscle strength and balance, which indirectly affects fracture risk by reducing the likelihood of falls.
Vitamin D deficiency has reached epidemic proportions globally, affecting an estimated one billion people worldwide. This widespread deficiency stems from limited sun exposure due to indoor lifestyles, use of sunscreen, geographic location, and dietary factors. The deficiency is particularly concerning because it significantly increases the risk of osteoporosis, fractures, and other bone-related disorders. It is important to get enough vitamin D to support bone health and overall well-being, and vitamin D supplements can help those at risk of deficiency achieve adequate levels.
The body can synthesize vitamin D when skin is exposed to UVB radiation from sunlight, but this natural production is influenced by factors such as skin pigmentation, age, season, latitude, and time of day. Vitamin D from sunlight is a key source for most people, and sunshine exposure is essential for vitamin D synthesis, especially during spring and early summer. For many people, especially those living in northern climates or with limited sun exposure, dietary sources and supplementation become essential for maintaining adequate vitamin D levels.
Dietary sources of vitamin D are limited, so supplementation is often recommended for those at risk of deficiency. Vitamin D supplements, including both D2 and D3 forms, are widely available and can help individuals meet their daily needs. Achieving all the vitamin D required for optimal health often involves a combination of sun exposure, food sources, and a daily supplement if necessary.

Beyond the Basics: Other Essential Bone Nutrients
Vitamin K: The Bone Protein Activator
Vitamin K plays a crucial but often overlooked role in bone health through its involvement in the production and activation of osteocalcin, a protein that helps bind calcium to the bone matrix. Without adequate vitamin K, osteocalcin cannot function properly, leading to impaired bone mineralization and increased fracture risk. In addition to its role in bone health, vitamin K is essential for blood clotting, helping to prevent excessive bleeding by supporting the blood clotting process.
There are two main forms of vitamin K: K1 (phylloquinone) found primarily in leafy green vegetables, and K2 (menaquinone) found in fermented foods and produced by gut bacteria. Vitamin K can be found in most foods, including fortified cereals, which can help individuals meet their daily requirements. Both forms contribute to bone health, but K2 appears to be particularly effective for bone and cardiovascular health.
Research suggests that vitamin K deficiency may be more common than previously thought, especially among older adults who may have reduced dietary intake of leafy greens or impaired gut bacteria production. Certain medications, particularly blood thinners, can also interfere with vitamin K metabolism.
The relationship between vitamin K and bone health is particularly important for postmenopausal women, who face accelerated bone loss due to declining estrogen levels. Studies have shown that adequate vitamin K intake can help slow bone loss and reduce fracture risk in this population.
Magnesium: The Metabolic Regulator
Magnesium serves as a cofactor for numerous enzymes involved in bone metabolism and is essential for converting vitamin D into its active form. Approximately 60% of the body's magnesium is stored in bones, where it contributes to bone structure and helps regulate calcium and phosphorus metabolism.
Magnesium deficiency can impair parathyroid hormone function, which regulates calcium levels in the blood and bones. This disruption can lead to altered calcium metabolism and compromised bone health, even when calcium and vitamin D intake appears adequate.
Modern diets often fall short in magnesium content due to soil depletion, food processing, and reduced consumption of magnesium-rich foods like whole grains, nuts, seeds, and leafy greens. Stress, certain medications, and medical conditions can also increase magnesium requirements or deplete magnesium stores.
The optimal ratio of calcium to magnesium intake is debated, but many experts suggest a ratio of approximately 2:1 or 3:1 (calcium to magnesium). This balance helps ensure that both minerals can perform their bone-supporting functions without interfering with each other's absorption or metabolism.
Vitamin C: The Collagen Builder
Vitamin C is essential for collagen synthesis, a protein that provides the flexible framework upon which bone minerals are deposited. Collagen makes up about 90% of the organic bone matrix, making vitamin C crucial for bone formation and repair. In addition to supporting collagen synthesis, vitamin C is also essential for maintaining healthy connective tissue in joints.
Beyond its role in collagen production, vitamin C functions as a powerful antioxidant that protects bone cells from oxidative damage and supports the differentiation of bone-forming cells. It also enhances the absorption of non-heme iron, which plays a role in collagen synthesis.
Vitamin C deficiency, while rare in developed countries, can lead to impaired bone formation and increased fracture risk. Even subclinical deficiencies may compromise optimal bone health, making adequate vitamin C intake important for bone maintenance throughout life.
Smoking significantly depletes vitamin C levels and is associated with increased fracture risk and delayed bone healing. This provides another compelling reason for smokers to quit and highlights the importance of adequate vitamin C intake for bone health.

The Science of Bone Remodeling
Understanding Bone Dynamics
Bone tissue is in a constant state of renewal through a process called remodeling, where old bone tissue is removed by cells called osteoclasts and new bone tissue is formed by cells called osteoblasts. This process allows bones to repair microscopic damage, adapt to mechanical stress, and maintain optimal strength throughout life.
The bone remodeling cycle typically takes about 3-6 months to complete and is influenced by mechanical stress, hormones, growth factors, and nutritional status. When nutrition is optimal and mechanical stress is appropriate, bone formation equals or exceeds bone resorption, maintaining or increasing bone mass.
As we age, this balance gradually shifts toward greater bone resorption than formation, leading to progressive bone loss. This age-related bone loss accelerates significantly after menopause in women due to declining estrogen levels, which normally help maintain the bone remodeling balance.
Understanding this dynamic process helps explain why consistent, long-term nutritional support is essential for bone health. Short-term dietary improvements may not immediately impact bone density measurements, but they contribute to the ongoing remodeling process that determines future bone strength.
Hormonal Influences on Bone Health
Hormones play a crucial role in bone metabolism, with estrogen, testosterone, parathyroid hormone, calcitonin, and growth hormone all influencing bone formation and resorption. Nutritional status can significantly impact hormone production and sensitivity, creating another pathway through which diet affects bone health. Hormonal imbalances, such as those occurring during menopause or due to certain medical conditions, can put individuals at greater risk for bone loss and osteoporosis.
Estrogen deficiency, whether due to menopause, eating disorders, or excessive exercise, dramatically accelerates bone loss by increasing osteoclast activity and decreasing calcium absorption. Adequate nutrition, particularly calcium, vitamin D, and phytoestrogens from plant foods, can help mitigate some of these effects.
Parathyroid hormone regulates calcium levels in the blood by increasing calcium absorption from the intestines, reducing calcium excretion by the kidneys, and stimulating calcium release from bones when blood calcium levels are low. Chronic elevation of parathyroid hormone due to calcium or vitamin D deficiency can lead to excessive bone loss.
Growth hormone and insulin-like growth factor-1 (IGF-1) promote bone formation and are influenced by protein intake, overall caloric intake, and specific nutrients like zinc and vitamin D. Maintaining adequate nutrition supports optimal hormone production and bone health throughout life.
Dietary Sources of Bone-Supporting Nutrients
Calcium-Rich Foods
While dairy products are often emphasized as primary calcium sources, many other foods provide significant amounts of this essential mineral. Dark leafy greens like kale, collard greens, and bok choy offer highly bioavailable calcium along with other bone-supporting nutrients like vitamin K and magnesium.
Canned fish with soft bones, such as sardines and salmon, provide not only calcium but also vitamin D and omega-3 fatty acids that support bone health. Almonds, sesame seeds, and tahini are excellent plant-based calcium sources that also provide healthy fats and protein.
Fortified foods, including plant-based milks, orange juice, and cereals, can significantly contribute to calcium intake, especially for individuals following vegetarian or vegan diets. These products often have added vitamin D to enhance calcium absorption. However, it’s important to check labels for calcium content and choose products fortified with calcium carbonate or calcium citrate for optimal absorption.
Traditional foods from various cultures often provide excellent calcium sources, such as tofu made with calcium sulfate, bone broth, and fermented dairy products. These foods often provide calcium in combination with other nutrients that enhance absorption and utilization.
Vitamin D Sources
Natural dietary sources of vitamin D are limited, with fatty fish like salmon, mackerel, and sardines being among the best sources. Egg yolks from pasture-raised chickens and mushrooms exposed to UV light also provide modest amounts of vitamin D.
Fortified foods play a crucial role in vitamin D intake, particularly fortified milk, plant-based milk alternatives, cereals, and some yogurts. The amount of fortification varies by product and country, making label reading important for tracking vitamin D intake.
Cod liver oil provides concentrated amounts of both vitamin D and vitamin A, though it should be used carefully to avoid vitamin A toxicity. Modern fish oil supplements often provide vitamin D without the high vitamin A content of traditional cod liver oil.
For most people, especially those with limited sun exposure, vitamin D supplementation becomes necessary to achieve optimal blood levels. The form of supplementation (D2 vs. D3) and dosing schedules can affect effectiveness and should be tailored to individual needs and blood levels. Dietary supplements, including vitamin D supplements, are especially important for individuals who cannot meet their vitamin D needs through food and sunlight alone, as recommended by authoritative sources such as the NIH Office of Dietary Supplements.
Plant-Based Bone Health
Plant-based diets can absolutely support excellent bone health when properly planned to include adequate amounts of calcium, vitamin D, vitamin K, and other bone-supporting nutrients. Many plant foods provide these nutrients in highly bioavailable forms along with additional compounds that support bone health. In addition, plant-based diets can help keep joints healthy by supplying essential nutrients such as vitamin C, leafy greens, and other vitamins and minerals important for joint and bone function.
Leafy greens not only provide calcium and vitamin K but also contain compounds like magnesium, potassium, and vitamin C that support bone metabolism. The alkalizing effect of fruits and vegetables may also help preserve bone mineral content by reducing acid load on the kidneys.
Soy foods, particularly those made with calcium coagulants, provide both calcium and isoflavones that may help maintain bone density, especially in postmenopausal women. The bone-protective effects of soy appear to be most pronounced in populations with lifelong consumption patterns.
Nuts, seeds, and legumes provide not only calcium and magnesium but also protein and healthy fats that support overall health and bone metabolism. The fiber content of plant foods also supports gut health, which may influence nutrient absorption and bone health through the gut-bone axis.
Age-Specific Bone Health Considerations
Childhood and Adolescence: Building Peak Bone Mass
The period from birth through the late twenties represents the most critical time for building bone mass, with approximately 90% of peak bone mass achieved by age 18 in girls and age 20 in boys. Nutritional inadequacies during this period can have lifelong consequences for bone health and fracture risk.
Calcium requirements are highest during adolescence, when rapid bone growth occurs. However, surveys consistently show that many teenagers, particularly girls, fall short of recommended calcium intakes. This shortfall often coincides with the replacement of milk with soft drinks and increased consumption of processed foods.
Vitamin D deficiency is increasingly common among children and adolescents, particularly those with darker skin, limited outdoor activity, or exclusive breastfeeding without vitamin D supplementation. This deficiency can lead to rickets in severe cases and suboptimal bone development in milder cases.
The eating behaviors established during childhood and adolescence often persist into adulthood, making this period crucial for developing healthy dietary patterns that support lifelong bone health. Family meals, school nutrition programs, and education about bone health can have lasting impacts on bone health trajectories.
Adult Years: Maintaining Bone Health
During the adult years, particularly from ages 30-50, the focus shifts from building bone mass to maintaining the peak bone mass achieved during youth. This period often coincides with career building, family responsibilities, and lifestyle changes that can impact bone health.
Pregnancy and breastfeeding create increased nutritional demands, particularly for calcium and vitamin D. The developing fetus and nursing infant will extract these nutrients from maternal stores if dietary intake is inadequate, potentially compromising maternal bone health.
Regular weight-bearing exercise becomes increasingly important during the adult years to maintain bone density and strength. Maintaining a healthy weight is also crucial, as it helps reduce stress on bones and joints, supporting overall skeletal health and lowering the risk of fractures. The combination of proper nutrition and exercise provides synergistic benefits that exceed what either intervention can achieve alone.
Lifestyle factors such as smoking, excessive alcohol consumption, and chronic stress can accelerate bone loss during the adult years. Addressing these factors while maintaining optimal nutrition helps preserve bone health for the decades ahead.

Menopause and Beyond: Protecting Against Bone Loss
Menopause marks a critical transition period for bone health, with estrogen decline leading to accelerated bone loss that can result in a 20% reduction in bone density within the first five years after menopause. This period requires heightened attention to bone-supporting nutrition and lifestyle factors. Postmenopausal women face an increased risk of osteoporosis and bone fractures due to these changes.
Calcium and vitamin D requirements increase after menopause due to decreased absorption efficiency and increased bone turnover. Many postmenopausal women require supplementation to achieve optimal intake levels, particularly if dietary sources are inadequate.
The risk-benefit profile of hormone replacement therapy for bone health continues to evolve, making nutritional and lifestyle interventions increasingly important for bone protection. Plant-based phytoestrogens may provide some bone-protective benefits with fewer risks than synthetic hormones.
Regular bone density testing becomes important after menopause to monitor bone health and guide treatment decisions. Nutritional interventions can help slow bone loss and reduce fracture risk, even in individuals with existing osteoporosis.
Supplementation Strategies and Considerations
When Supplements Become Necessary
While obtaining nutrients from whole foods is generally preferable, certain circumstances make supplementation necessary or beneficial for optimal bone health. These situations include limited dietary intake, absorption issues, increased requirements, or specific health conditions that affect nutrient status.
Vitamin D supplementation is often necessary regardless of diet quality, particularly for individuals with limited sun exposure, darker skin pigmentation, or living in northern climates. Blood testing can help determine individual vitamin D status and guide appropriate supplementation levels.
A calcium supplement may be beneficial for individuals with lactose intolerance, vegan diets, or other dietary restrictions that limit calcium-rich food consumption. However, supplementation should complement, not replace, dietary sources of calcium whenever possible. It is important to use a calcium supplement appropriately, as excessive intake can increase the risk of kidney stones.
Older adults often have increased supplement needs due to decreased absorption efficiency, medication interactions, and reduced dietary intake. Comprehensive evaluation of nutritional status helps guide appropriate supplementation strategies for this population.
Choosing Quality Supplements
The supplement industry is vast and variable in quality, making informed selection crucial for safety and effectiveness. Third-party testing, reputable manufacturers, and appropriate certifications help ensure supplement quality and potency.
Calcium supplements come in various forms, with calcium citrate generally offering better absorption than calcium carbonate, particularly when taken without food. The total elemental calcium content and serving size should be considered when comparing products.
Vitamin D3 (cholecalciferol) is generally preferred over vitamin D2 (ergocalciferol) for supplementation due to better bioavailability and longer duration of action. The appropriate dose depends on individual vitamin D status, sun exposure, and other factors.
Combination supplements that include multiple bone-supporting nutrients can be convenient but may not provide optimal ratios or doses of individual nutrients. Single-nutrient supplements allow for more precise dosing based on individual needs and blood levels.
Timing and Absorption Optimization
The timing of supplement intake can significantly affect absorption and effectiveness. Calcium absorption is limited to about 500mg at one time, making divided doses more effective than single large doses for individuals requiring high calcium intake.
Taking calcium supplements with meals generally improves absorption, particularly for calcium carbonate which requires stomach acid for dissolution. Calcium citrate can be taken with or without food and may be better tolerated by individuals with low stomach acid production.
Vitamin D is fat-soluble and should be taken with meals containing some fat for optimal absorption. The timing of vitamin D supplementation is less critical than calcium, as vitamin D has a longer half-life in the body.
Certain nutrients can interfere with each other’s absorption when taken simultaneously. For example, calcium can reduce iron absorption, while high doses of zinc can interfere with copper absorption. Spacing supplements or taking them at different times can help minimize these interactions.
Additionally, when engaging in exercise, it is important to use proper footwear designed to absorb shock and protect your joints.

Lifestyle Factors That Support Bone Health
Exercise and Mechanical Stress
Weight-bearing and resistance exercises provide mechanical stress that stimulates bone formation and helps maintain bone density throughout life. The principle of "use it or lose it" applies strongly to bone health, with sedentary lifestyles contributing to accelerated bone loss.
High-impact activities like jumping, running, and dancing provide particularly strong bone-building signals, while resistance training helps maintain muscle mass that supports bone health. Even moderate activities like walking can provide bone benefits, especially for older adults.
The timing of exercise during youth is particularly important for maximizing peak bone mass, but exercise benefits bone health at any age. Older adults should focus on exercises that improve balance and coordination to reduce fall risk, as falls are the primary cause of fractures in this population.
Progressive overload principles apply to bone health just as they do to muscle building. Gradually increasing the intensity, duration, or frequency of weight-bearing activities helps continue providing bone-building stimulus over time.
Sleep and Stress Management
Quality sleep is essential for bone health, as growth hormone release and bone formation occur primarily during sleep. Chronic sleep deprivation can disrupt these processes and contribute to accelerated bone loss over time.
Chronic stress elevates cortisol levels, which can suppress bone formation and increase bone resorption. Stress management techniques such as meditation, yoga, and regular relaxation practices can help mitigate these negative effects on bone health.
The relationship between mental health and bone health is increasingly recognized, with depression and anxiety associated with increased fracture risk. Addressing mental health concerns as part of comprehensive bone health management may provide additional benefits.
Work-life balance and social connections also influence bone health indirectly through their effects on stress levels, physical activity, and dietary choices. A holistic approach to health that includes attention to these factors supports optimal bone health outcomes.
Environmental and Lifestyle Toxins
Smoking is one of the most significant modifiable risk factors for poor bone health, directly impairing bone formation while increasing bone resorption. The negative effects of smoking on bone health begin within years of smoking initiation and can persist for years after quitting.
Excessive alcohol consumption interferes with bone metabolism by affecting hormone levels, nutrient absorption, and bone cell function. Moderate alcohol consumption may have neutral or even slightly positive effects on bone density, but heavy drinking is clearly detrimental.
Environmental toxins such as heavy metals, pesticides, and industrial chemicals can accumulate in bone tissue and interfere with normal bone metabolism. Minimizing exposure to these toxins through dietary choices, water filtration, and lifestyle modifications supports optimal bone health.
Certain medications, including corticosteroids, proton pump inhibitors, and some anticonvulsants, can negatively impact bone health. Working with healthcare providers to minimize these effects through appropriate monitoring, supplementation, or alternative treatments is important for individuals requiring long-term medication use. When considering sun exposure for vitamin D synthesis, it is also essential to balance this with the use of sunscreen and other protective measures to prevent skin cancer.

Special Populations and Bone Health
Athletes and High-Performance Individuals
Athletes have unique bone health considerations due to high mechanical stress on bones, increased nutrient requirements, and potential risk factors such as low body weight or menstrual irregularities. The combination of appropriate nutrition and training can optimize bone health in athletic populations.
Female athletes are at particular risk for bone health issues due to the potential for low energy availability, menstrual dysfunction, and eating disorders. The female athlete triad (low energy availability, menstrual dysfunction, and low bone density) requires comprehensive intervention including nutritional rehabilitation.
Endurance athletes may have increased calcium and vitamin D requirements due to losses through sweat and increased turnover. Sports drinks and foods consumed during training should be considered as potential sources of bone-supporting nutrients.
The timing of nutrient intake around training sessions may influence bone adaptation to exercise. Consuming calcium and protein after exercise may help optimize the bone-building response to mechanical stress.
Individuals with Chronic Diseases
Chronic diseases such as inflammatory bowel disease, celiac disease, and chronic kidney disease can significantly impact bone health through effects on nutrient absorption, metabolism, or excretion. These conditions require specialized nutritional approaches to maintain bone health.
Autoimmune diseases and their treatments often involve corticosteroid medications that accelerate bone loss. Proactive bone health management, including optimized nutrition and appropriate supplementation, becomes crucial for these individuals.
Gastrointestinal disorders can impair absorption of bone-supporting nutrients, making higher intake levels or specialized supplement forms necessary. Working with knowledgeable healthcare providers helps ensure appropriate monitoring and intervention.
Cancer survivors may have bone health challenges related to treatment effects, hormonal changes, or medication side effects. Comprehensive bone health assessment and management should be part of survivorship care planning.
Vegetarian and Vegan Populations
Plant-based diets can absolutely support excellent bone health when properly planned, but require attention to specific nutrients that may be less abundant or bioavailable from plant sources. Calcium, vitamin D, vitamin B12, and zinc are nutrients of particular concern.
The bioavailability of calcium from plant sources varies significantly, with leafy greens generally providing highly absorbable calcium while some foods contain compounds that inhibit calcium absorption. Understanding these differences helps optimize calcium intake from plant sources.
Vitamin B12 deficiency, common in vegans who don't supplement, may indirectly affect bone health through its effects on homocysteine metabolism. Regular B12 supplementation or monitoring is essential for long-term bone health in vegan populations.
The alkalizing effect of plant-based diets may provide bone health benefits by reducing the acid load that can contribute to bone mineral loss. This potential benefit highlights the importance of fruits and vegetables for bone health regardless of dietary pattern.
Future Directions in Bone Health Research
Emerging Nutrients and Compounds
Research continues to identify new nutrients and compounds that may support bone health beyond the traditional focus on calcium and vitamin D. Vitamin K2, boron, silicon, and various plant compounds are gaining attention for their potential bone health benefits.
The gut microbiome's influence on bone health is an emerging area of research, with studies suggesting that gut bacteria may influence calcium absorption, immune function, and inflammatory processes that affect bone health. Prebiotic and probiotic interventions may become important tools for bone health optimization.
Collagen supplementation is gaining popularity for bone health, though research is still emerging on its effectiveness compared to ensuring adequate vitamin C and protein intake for natural collagen synthesis.
Advanced understanding of bone metabolism at the cellular and molecular level may lead to more targeted nutritional interventions that optimize specific pathways involved in bone formation and resorption.
Personalized Nutrition for Bone Health
Genetic testing is beginning to reveal individual variations in nutrient metabolism that may influence optimal intake levels for bone health. Polymorphisms in genes related to vitamin D metabolism, calcium absorption, and bone protein synthesis may guide personalized nutrition recommendations.
Biomarker assessment beyond traditional bone density measurements may help identify individuals at risk for bone health problems before significant bone loss occurs. Markers of bone turnover, inflammation, and nutrient status can guide early intervention strategies.
The integration of wearable technology and continuous monitoring may provide new insights into how daily activities, stress levels, and dietary choices affect bone metabolism in real-time.
Machine learning and artificial intelligence applications may help predict bone health outcomes and optimize intervention strategies based on individual characteristics and risk factors.
Public Health Implications
The economic burden of osteoporotic fractures continues to grow as populations age, making prevention through nutrition and lifestyle interventions increasingly important from a public health perspective.
Food fortification policies and programs may need to evolve to address changing dietary patterns and ensure adequate intake of bone-supporting nutrients across populations.
Educational initiatives that promote bone health awareness during youth may have significant long-term benefits for population bone health and healthcare costs.
Integration of bone health considerations into broader healthy aging and chronic disease prevention programs may provide synergistic benefits for multiple health outcomes.

Conclusion: Building a Foundation for Lifelong Bone Health
Optimal bone health represents a lifelong investment that pays dividends in mobility, independence, and quality of life throughout the aging process. While genetics certainly influence bone health outcomes, nutritional and lifestyle factors provide powerful tools for optimizing bone health regardless of genetic predisposition.
The foundation of bone health nutrition rests on adequate intake of calcium, vitamin D, and supporting nutrients including vitamin K, magnesium, vitamin C, and protein. However, the most effective approach goes beyond individual nutrients to encompass dietary patterns, lifestyle factors, and comprehensive health management that supports the complex biological processes underlying bone health.
Understanding that bone health is not just about preventing osteoporosis, but about maintaining the structural foundation that supports an active, vibrant life, helps motivate the consistent attention that optimal bone health requires. The habits established today directly influence bone health outcomes decades in the future.
The good news is that it's never too late to begin supporting bone health through improved nutrition and lifestyle choices. While the greatest benefits come from lifelong attention to bone health, research consistently shows that interventions at any age can help slow bone loss, reduce fracture risk, and improve quality of life.
The investment in bone health nutrition and lifestyle is an investment in future independence, mobility, and vitality. By understanding the science behind bone health and implementing evidence-based strategies, individuals can take control of their bone health destiny and build a foundation for lifelong strength and resilience.
Whether you're a parent supporting your child's peak bone mass development, an adult maintaining bone health through busy middle years, or an older adult working to preserve bone strength and reduce fracture risk, the principles of bone health nutrition provide a roadmap for optimizing this crucial aspect of overall health and longevity.












