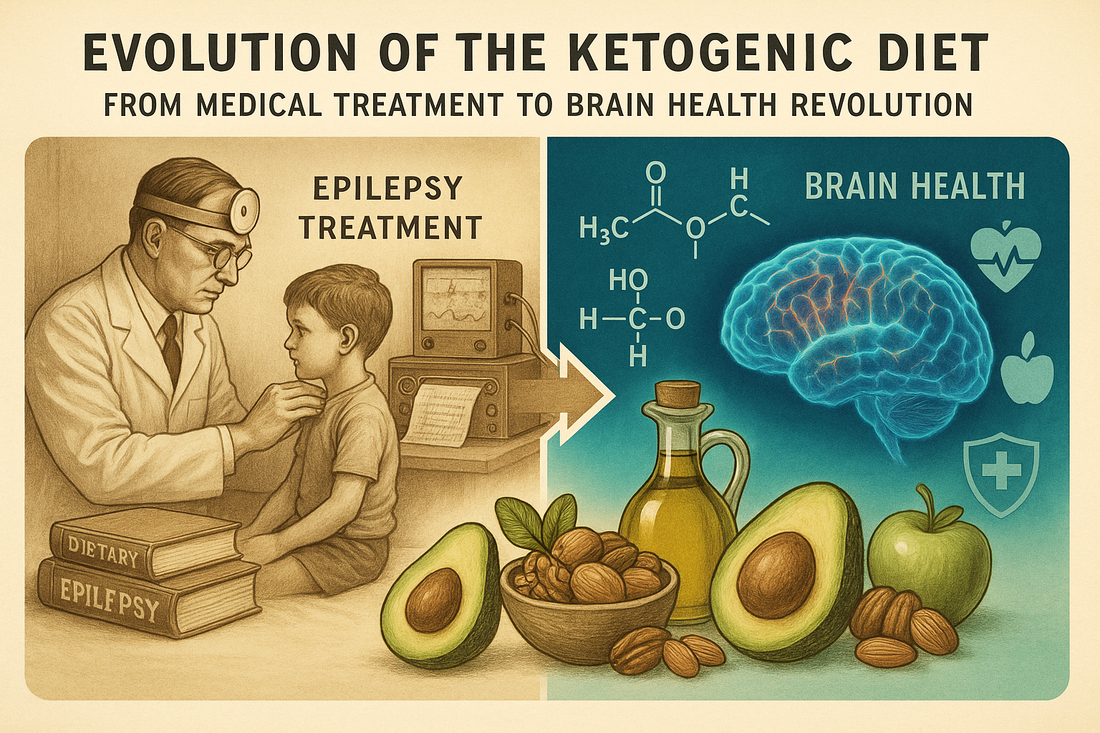
In the bustling corridors of Johns Hopkins Hospital in the 1920s, a revolutionary discovery was taking shape that would transform our understanding of nutrition's role in neurological health. What began as a desperate search for seizure treatments in children has evolved into one of today's most studied dietary approaches for brain health and overall wellness. The ketogenic diet's remarkable journey from medical necessity to mainstream phenomenon reveals the profound connection between what we eat and how our brains function.
A Medical Marvel Born from Necessity
The ketogenic diet emerged during an era when medical options for childhood epilepsy were severely limited. In the early 20th century, physicians had observed a curious phenomenon: children with severe epilepsy often experienced dramatic reductions in seizures during periods of fasting. While fasting provided relief, it obviously couldn't be sustained long-term without serious health consequences.
Dr. Russell Wilder at the Mayo Clinic coined the term "ketogenic diet" in 1921, but it was Dr. Hugh Conklin who first systematically explored the therapeutic potential of fasting for epilepsy. Conklin noticed that his patients' seizures often decreased significantly during periods when they consumed little to no food. This observation led to a critical question: could the benefits of fasting be maintained through dietary manipulation rather than complete food restriction?
The answer came through understanding the body's metabolic response to carbohydrate restriction. When glucose from carbohydrates becomes unavailable, the liver begins breaking down fats into molecules called ketones. These ketones can cross the blood-brain barrier and serve as an alternative fuel source for brain cells. The ketogenic diet was specifically designed to trigger this metabolic state, called ketosis, while still providing adequate nutrition for growing children.

The Science Behind Seizure Control
The mechanism by which the ketogenic diet reduces seizures involves complex changes in brain metabolism and neurotransmitter function. When brain cells use ketones instead of glucose for energy, several neurological changes occur that make seizures less likely to develop and spread.
Ketones appear to stabilize neuronal membranes, making brain cells less excitable and reducing the electrical storms that characterize seizures. The diet also influences neurotransmitter production, increasing levels of GABA, the brain's primary inhibitory neurotransmitter, while modulating glutamate, an excitatory neurotransmitter often involved in seizure activity.
Additionally, the ketogenic diet affects mitochondrial function within brain cells. Mitochondria are the cellular powerhouses responsible for energy production, and many neurological disorders involve mitochondrial dysfunction. Ketones provide a more efficient fuel source for mitochondria, potentially improving cellular energy production and reducing oxidative stress that can contribute to seizure activity.
The anti-inflammatory effects of ketosis also play a role in seizure control. Chronic inflammation in the brain can increase seizure susceptibility, and the ketogenic diet has been shown to reduce inflammatory markers while promoting the production of anti-inflammatory compounds.

Clinical Success and Modern Applications
The clinical results of the ketogenic diet for pediatric epilepsy have been consistently impressive across nearly a century of use. Studies consistently show that approximately 50% of children with drug-resistant epilepsy experience a 50% or greater reduction in seizures when following a properly implemented ketogenic diet. Even more remarkably, about 15-20% of children become completely seizure-free.
These results are particularly significant because the children who typically receive ketogenic diet therapy have already failed to respond to multiple anti-seizure medications. For families who have exhausted pharmaceutical options, the diet often represents hope when conventional medicine has reached its limits.
Modern implementation of the ketogenic diet for epilepsy involves careful medical supervision, typically requiring hospitalization for initiation and ongoing monitoring by specialized medical teams. The medical version is far more restrictive than popular ketogenic diets, often requiring precise ratios of fats to carbohydrates and proteins, usually ranging from 3:1 to 4:1 ratios by weight.
The diet's success in treating epilepsy has led to the development of several variations designed to be more tolerable while maintaining therapeutic effectiveness. The Modified Atkins Diet, the Low Glycemic Index Treatment, and Medium Chain Triglyceride diets all represent efforts to capture the seizure-controlling benefits of ketosis while improving adherence and quality of life.

Expanding Horizons: From Epilepsy to Brain Health
The remarkable neuroprotective effects observed in epilepsy treatment have sparked intense research into the ketogenic diet's potential for other neurological conditions. Scientists began asking whether the brain-protective mechanisms that reduce seizures might also benefit other forms of neurological dysfunction.
Alzheimer's disease research has shown particular promise, with studies suggesting that the brain's reduced ability to use glucose effectively in Alzheimer's might be compensated by providing ketones as an alternative fuel. Some researchers refer to Alzheimer's as "type 3 diabetes" due to the brain's insulin resistance, and ketones bypass this glucose utilization problem entirely.
Parkinson's disease research has explored whether ketones might protect the dopamine-producing neurons that are progressively lost in this condition. Preliminary studies suggest that ketogenic approaches might slow disease progression and improve motor symptoms, though more research is needed to confirm these effects.
Traumatic brain injury represents another area of intense interest. The brain's energy demands increase dramatically after injury, and its ability to use glucose effectively is often compromised. Ketones provide an alternative energy source that might support healing and reduce secondary brain damage.
Multiple sclerosis, amyotrophic lateral sclerosis (ALS), and even certain types of brain tumors are being investigated as potential targets for ketogenic interventions. The common thread connecting these diverse conditions is the potential for ketones to provide neuroprotection through improved cellular energy production and reduced inflammation.
The Metabolic Revolution
Understanding the ketogenic diet's neurological benefits has revolutionized our appreciation of metabolism's role in brain health. This knowledge has implications far beyond treating specific diseases, extending to cognitive enhancement, mental health, and healthy aging.
Research suggests that periodic ketosis might provide cognitive benefits even in healthy individuals. Studies have shown improvements in memory, focus, and mental clarity during ketosis, leading to interest in using ketogenic approaches for cognitive enhancement and academic performance.
Mental health applications are also being explored, with some research suggesting that ketogenic diets might benefit certain types of depression, anxiety, and bipolar disorder. The metabolic and neurotransmitter changes associated with ketosis appear to have mood-stabilizing effects that complement traditional psychiatric treatments.
The relationship between metabolic health and brain function has become increasingly clear through ketogenic diet research. Poor metabolic health, characterized by insulin resistance and chronic inflammation, appears to negatively affect brain function across multiple domains. Conversely, the metabolic improvements associated with ketogenic diets often correspond with enhanced cognitive function.
Modern Challenges and Considerations
While the ketogenic diet's medical applications continue to expand, implementing it safely and effectively requires careful consideration of individual circumstances and potential risks. The medical ketogenic diet used for epilepsy involves strict supervision, regular monitoring of blood chemistry, and careful attention to nutritional adequacy.
Potential side effects can include kidney stones, bone demineralization, growth delays in children, and various gastrointestinal issues. These risks underscore the importance of medical supervision when using ketogenic approaches therapeutically rather than recreationally.
The difference between medical ketogenic diets and popular ketogenic diets for weight loss is significant. Medical versions require precise macronutrient ratios, careful monitoring, and often supplementation to prevent nutritional deficiencies. Popular versions are typically less restrictive but may not achieve the same therapeutic benefits.
Individual variation in response to ketogenic diets is substantial, with some people experiencing dramatic benefits while others see minimal effects or develop side effects. Genetic factors, gut microbiome composition, and underlying health conditions all influence individual responses to ketogenic interventions.

The Future of Therapeutic Nutrition
The ketogenic diet's journey from epilepsy treatment to broad neurological therapy represents a paradigm shift in how we view nutrition's therapeutic potential. This evolution has opened new avenues for treating neurological conditions through dietary intervention rather than exclusively through pharmaceutical approaches.
Current research is exploring ways to optimize ketogenic approaches for different conditions, developing more targeted interventions that maximize benefits while minimizing side effects. This includes investigating specific types of ketones, optimal timing of ketogenic periods, and combination approaches that integrate ketogenic diets with other therapeutic modalities.
The development of exogenous ketone supplements represents another frontier, potentially allowing people to experience some benefits of ketosis without strict dietary restrictions. These supplements might provide a bridge between full ketogenic diets and conventional approaches, offering flexibility while maintaining therapeutic potential.
Personalized medicine approaches are being developed to identify who is most likely to benefit from ketogenic interventions. Genetic testing, metabolic profiling, and biomarker analysis may eventually allow clinicians to predict individual responses and customize ketogenic protocols accordingly.
Lessons for Modern Medicine
The ketogenic diet's success story offers important lessons about the relationship between nutrition and health that extend far beyond neurological conditions. It demonstrates that food can indeed be medicine when applied with scientific rigor and appropriate medical supervision.
The diet's history also illustrates the value of observational medicine and clinical intuition. The original observation that fasting reduced seizures came from careful clinical observation rather than laboratory research, highlighting the importance of paying attention to real-world patient experiences.
Perhaps most importantly, the ketogenic diet's evolution shows how understanding underlying mechanisms can transform isolated observations into systematic therapeutic approaches. By understanding why fasting helped seizures, researchers could develop sustainable dietary interventions that captured the same benefits.
Implications for Public Health
The broader implications of ketogenic diet research extend to public health approaches for preventing neurological decline and supporting cognitive health throughout life. As populations age and neurodegenerative diseases become more prevalent, nutritional approaches for brain health take on increasing importance.
The research suggests that metabolic health and brain health are intimately connected, with implications for how we approach education, workplace productivity, and healthy aging. Understanding these connections might inform public health strategies that use nutritional interventions to support cognitive function and prevent neurological decline.
The ketogenic diet's medical origins also highlight the potential for other therapeutic dietary approaches. If dramatic neurological benefits can be achieved through dietary manipulation, what other conditions might respond to targeted nutritional interventions?
A Legacy of Innovation
From its humble beginnings as a treatment for childhood epilepsy to its current status as a subject of intense scientific investigation, the ketogenic diet represents one of medicine's most remarkable nutritional success stories. The journey from Johns Hopkins Hospital in the 1920s to modern research laboratories worldwide illustrates how medical innovation can emerge from careful observation, scientific curiosity, and willingness to challenge conventional approaches.
The diet's evolution from a last-resort treatment to a mainstream therapeutic option demonstrates the power of persistent research and clinical application. Each generation of researchers has built upon previous knowledge, gradually expanding our understanding of how nutrition affects brain function and overall health.
Today, as we face increasing rates of neurological disorders and seek new approaches to supporting brain health throughout life, the ketogenic diet's medical origins provide both inspiration and practical guidance. The principles discovered through treating childhood epilepsy continue to inform new therapeutic approaches, reminding us that sometimes the most profound medical advances come from the simplest observations about how our bodies respond to what we eat.
The story of the ketogenic diet is ultimately a story about the intersection of necessity, observation, and scientific rigor. It reminds us that breakthrough medical treatments often emerge from unexpected sources and that the path from clinical observation to therapeutic application requires patience, persistence, and open-minded investigation. As research continues to expand our understanding of nutrition's role in neurological health, the ketogenic diet's remarkable journey from seizure treatment to brain health revolution serves as a compelling example of medicine's potential to transform lives through innovative thinking and careful application of scientific principles.